ITB syndrome in long-distance runners and walkers
What is an ITB syndrome?
Your iliotibial band is a long thin band of fascia which runs down the outside of your thigh. It spans from the top of your hip and goes down to the side of your knee.
The iliotibial band friction syndrome (ITB syndrome) refers to an issue that often occurs to long-distance runners and walkers, where band inflames due to repetitive friction of the tendon band against your thigh bone (femur).
How commonly does ITB syndrome occur?
ITB syndrome is one of the most common causes of "Runner's Knee" and can account for up to 22% of overuse injuries in runners. It is also a common presentation in exercising adults, occurring in up to 15% of women and 7% of men (Falvey, et al. 2010)
It is caused by repeated use and pressure rather than a specific incident.
What causes the repetitive friction of the iliotibial band?
The repetitive friction of the ITB is precipitated by poor running biomechanics and underlying muscular imbalances. Fatigue of your side-gluteal muscle forces your ITB to compensate during running, thus increases pressure put through the side of your knee.
The most common muscle imbalances are from:
Weak hip/gluteal stabilises
Weak hip rotators
Weak inner quadriceps
Weak core muscles
Poor foot arch control
Other factors that can lead to poor running form:
Training in worn-out or unsuitable running shoes
A sudden increase in training
Excessive hill walking/running (especially downhill)
Poor running technique
You might feel these symptoms:
Sharp or burning pain just above the outer part of the knee
Pain over the pathway of the outer leg
Pain over the front and outside of the knee or thigh.
Pain that worsens with the continuance of running or other repetitive activities
Physios can do to help with treatment:
Good news! It is definitely treatable and on average takes 2-4 weeks to see a significant improvement! Our treatment involves:
First determine the cause: imbalance of muscles, weakness, or running technique
Reduce acute pain with soft tissue and joint mobilisations
Modify your current exercise program to fix the imbalances
Create an exercise program to reduce the risk of re-injury
What you can do for yourself?
You can self release your ITB using a form roller.
Roll up to your hip and down to your knee approx. x5 times
With your hands and legs supported on the ground like shown in the picture to ensure that only part of your body weight goes onto that form roller. Be gentle to start off with as it can be quite tender to do this.
Self release your ITB using a foam roller
Roll the foam roller up to your hip and down to your knee approximately 5 times.
With your hands and legs supported on the ground like shown in the picture to ensure that only part of your body weight goes onto that form roller. Be gentle to start off with as it can be quite tender to do this.
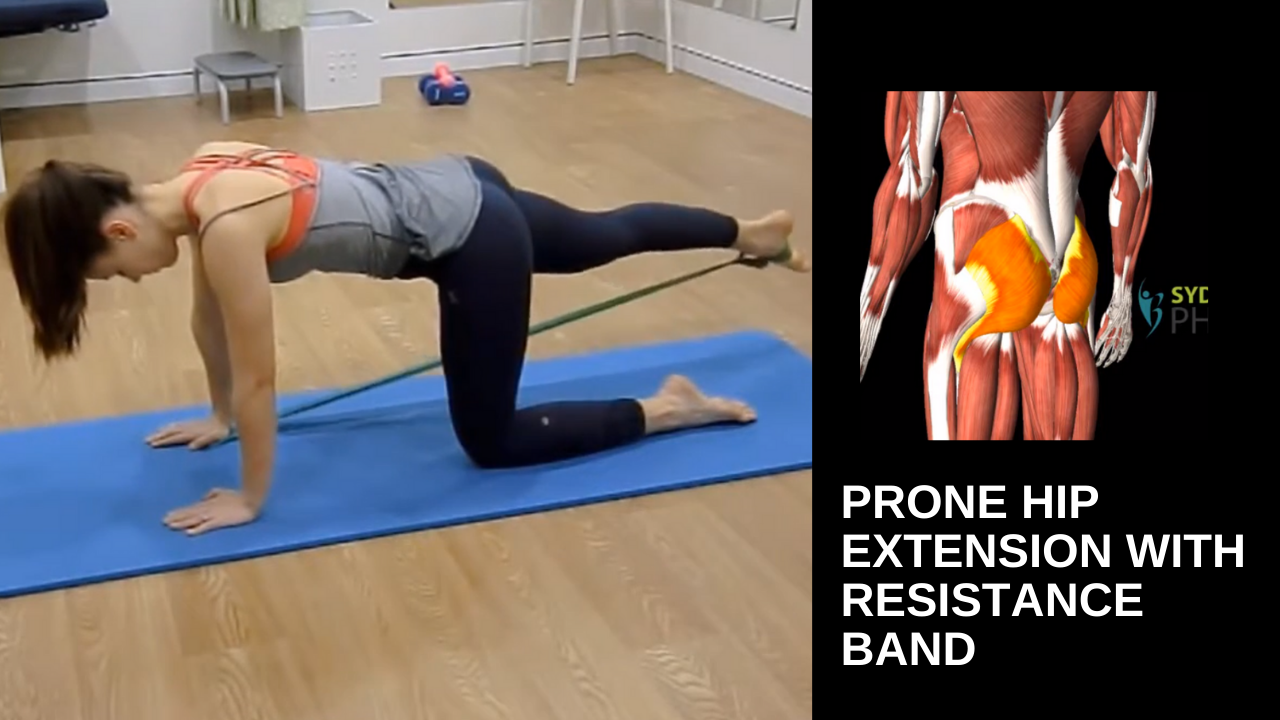
Resistance bands
Keeping your feet hip-width apart, making sure the bands are on quite a bit of a stretch. Place the band around your upper legs and perform squats (10 reps of 3 sets) to improve your hip strength and stability.
Ensure to keep your knees from going over your toes but not letting them collapse inwards. Keep them moving towards your outer toes.
Reference and evidence
Falvey, E., Clark,R., Franklyn‐Miller, A., Bryant, A., Briggs, C.,& McCrory, P. (2010). Iliotibial band syndrome: An examination of theevidence behind a number of treatment options. Scandinavian Journal ofMedicine & Science in Sports,20(4), 580-587.
Lavine R.Iliotibial band friction syndrome. Current Reviews in Musculoskeletal Medicine,2010; 3(1-4) :18–22
SchwellnusMP, Theunissen L, Noakes TD, Reinach SG. Anti-inflammatory andcombined anti-inflammatory/analgesic medication in the early management ofiliotibial band friction syndrome: A clinical trial. South-Africa MedicineJournal, 1991;79(10):602-6.